


Through our Pitch Your Pills campaign, the Seminole Prevention Coalition has compiled a toolkit of resources for you. Designed to increase awareness of the issue and to move our community to action this prescription drug abuse prevention toolkit is simple and yet effective.
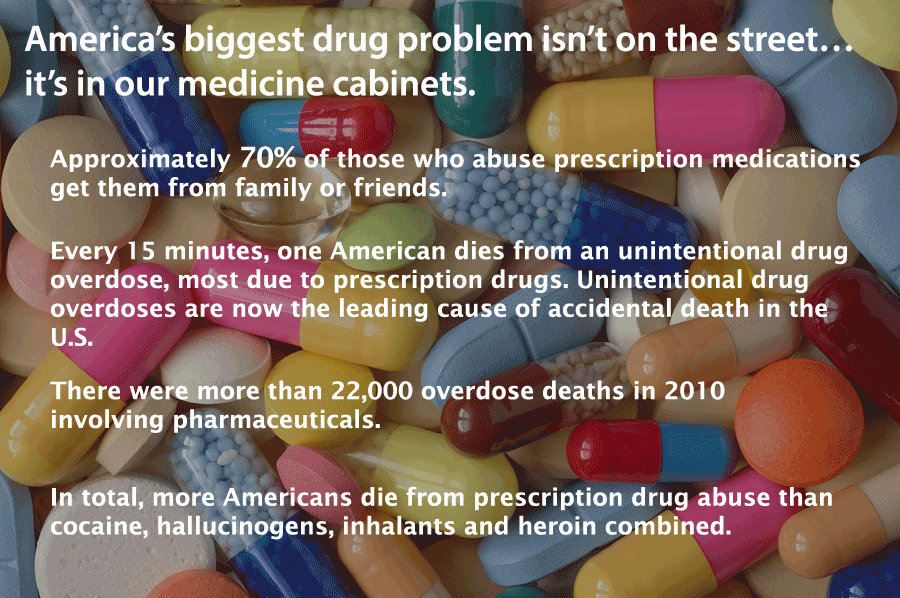
In 2011, doctors in the U.S. wrote 4.02 billion prescriptions for medication. Based on the current U.S. population that’s roughly 13 prescriptions for every man, woman, and child living in America.
When used as prescribed, prescription drugs are safe medications that help millions of people. However, improper storage and disposal practices have many health risks leading to increased drug abuse, environmental harm and accidental poisoning.
Learn how to prevent prescription drug abuse with the resources provided on this page and take action to end the prescription drug abuse epidemic today!

Parents are in an influential position to immediately help reduce teen access to prescription drugs because these drugs are found in the home. But how aware are you?
Think about this: would you know if some of your pills were missing?
From this day forward, make sure you can honestly answer, “yes.”

Teens abuse prescription drugs because they are easily accessible and either free or inexpensive. In fact, 64 percent of kids age 12 to 17 who have abused pain relievers say they got them from their friends or relatives, typically without their knowledge.
Approach securing your prescriptions the same way you would other valuables in your home, like jewelry or cash. There’s no shame in helping protect those items. The same holds true for your medications.
Learn about safe-guarding your prescriptions today.

Safely disposing of expired or unused prescription medications is a critical step in helping protect your teens. Here’s how to help safeguard your family and home, and decrease the opportunity for your teens or their friends to abuse your medications.
Prescription drug disposal facts
Talk to your teen and warn them that taking prescription medications without a doctor’s supervision can be just as dangerous and as potentially lethal as taking illicit drugs. For example, pain killers are made from opioids, the same substance as in heroin.
Keep medications hidden in your home and out of easily accessible places like the medicine cabinet. Also, remind parents and family members whose homes your teen visits to keep prescription medications out of reach, rather than in the medicine cabinet
Ask your healthcare provider if any medications prescribed for your family have a potential for abuse.
Take an inventory of Rx and OTC medications in your home. Pay attention to quantities.
If your child needs medications during school hours, speak with school officials about policies for distributing medications to students. If possible, personally take the medications to the school nurse. Make sure unused medications are returned to you.
Parents360 Medicine Abuse – This narrated slidecast addresses medicine abuse and the role parents can play in preventing and responding to this issue. Click on this link and the slidecast will open in a new window National Council on Patient Information and Education – (www.talkaboutrx.org) National Institute on Drug Abuse – (www.nida.nih.gov) Office of National Drug Control Policy –(www.whitehousedrugpolicy.gov) Parents. The Anti-Drug – (www.theantidrug.com) Partnership for a Drug-Free America – (www.drugfree.org) Stop Medicine Abuse The Ohio State University College of Pharmacy Generation Rx Initiative – (www.go.osu.edu/generationrx) Prescription and Over-the-Counter Drugs – A parent’s guide to the legal drugs kids are using and abusing. Tips for Safe Medicine Storage Prescription Drug Facts – Six easy lessons on Rx drug use trends among teens, slang terms used by abusers and steps you can take to secure your medicines. Prescription Drug Inventory Card – Keep track of your Rx meds with this simple chart. 10 Tips to Prevent Accidental Prescription Drug Overdose – FDA Consumer Health Information Prescription Drugs: Abuse and Addiction – NIDA Research Report Series Facts on Prescription and Over-The-Counter Drugs – Learn about prescription drug abuse and commonly abused prescription drugs. Drug Guide for Parents – Learn the facts to keep your teen safe. Pill Identifier – Worried about some capsules found in your teenager’s room? Use this website to identify unknown Rx meds by imprint, size, shape, or color.
A website created by the Consumer Healthcare Products Association – (www.stopmedicineabuse.org)

Aging and Health: You and Your Medicines
As you age, it is important to know about your medicines to avoid possible problems. As you get older you may be faced with more health conditions that you need to treat on a regular basis. It is important to be aware that more use of medicines and normal body changes caused by aging can increase the chance of unwanted or maybe even harmful drug interactions.
The more you know about your medicines and the more you talk with your health care professionals, the easier it is to avoid problems with medicines.
As you age, body changes can affect the way medicines are absorbed and used. For example, changes in the digestive system can affect how fast medicines enter the bloodstream. Changes in body weight can influence the amount of medicine you need to take and how long it stays in your body. The circulation system may slow down, which can affect how fast drugs get to the liver and kidneys. The liver and kidneys also may work more slowly affecting the way a drug breaks down and is removed from the body.
Because of these body changes, there is also a bigger risk of drug interactions for older adults. Drug-drug interactions happen when two or more medicines react with each other to cause unwanted effects. This kind of interaction can also cause one medicine to not work as well or even make one medicine stronger than it should be. For example, you should not take aspirin if you are taking a prescription blood thinner, such as Warfarin, unless your health care professional tells you to.
Drug-condition interactions happen when a medical condition you already have makes certain drugs potentially harmful. For example, if you have high blood pressure or asthma, you could have an unwanted reaction if you take a nasal decongestant.
Drug-food interactions result from drugs reacting with foods or drinks. In some cases, food in the digestive track can affect how a drug is absorbed. Some medicines also may affect the way nutrients are absorbed or used in the body.
Drug-alcohol interactions can happen when the medicine you take reacts with an alcoholic drink. For instance, mixing alcohol with some medicines may cause you to feel tired and slow your reactions.
It is important to know that many medicines do not mix well with alcohol. As you grow older, your body may react differently to alcohol, as well as to the mix of alcohol and medicines. Keep in mind that some problems you might think are medicine-related, such as loss of coordination, memory loss, or irritability, could be the result of a mix between your medicine and alcohol.
Talk to Your Health Care Professionals
It is important to go to all of your medical appointments and to talk to your team of health care professionals (doctors, pharmacists, nurses, or physician assistants) about your medical conditions, the medicines you take, and any health concerns you have.
It may help to make a list of comments, questions, or concerns before your visit or call to a health care professional. Also, think about having a close friend or relative come to your appointment with you if you are unsure about talking to your health care professional or would like someone to help you understand and/or remember answers to your questions.
Here are some other things to keep in mind:
– All Medicines Count: Tell your team of health care professionals about all the medicines you take, including prescription and over-the-counter medicines, such as pain relievers, antacids, cold medicines, and laxatives. Don’t forget to include eye drops, dietary supplements, vitamins, herbals, and topical medicines, such as creams and ointments.
– Keep in Touch with Your Doctors: If you regularly take a prescription medicine, ask your doctor to check how well it is working, whether you still need to take it, and, if so, whether there is anything you can do (like lowering fats in your diet or exercising more) to cut back or, in time, stop needing the medicine. Don’t stop taking the medicine on your own without first talking with your doctor.
– Medical History: Tell your health care professional about your medical history. The doctor will want to know if you have any food, medicine, or other allergies. He or she also will want to know about other conditions you have or had and how you are being treated or were treated for them by other doctors. It is helpful to keep a written list of your health conditions that you can easily share with your doctors. Your primary care doctor should also know about any specialist doctors you may see on a regular basis.
– Eating Habits: Mention your eating habits. If you follow or have recently changed to a special diet (a very low-fat diet, for instance, or a high-calcium diet), talk to your doctor about this. Tell your doctor how much coffee, tea, or alcohol you drink each day and whether you smoke. These things may make a difference in the way your medicine works. Tell your health professionals about your medical history and about all medicines or supplements you take.
– Recognizing and Remembering to Take Your Medicines: Let your health care professional know if you have trouble telling your medicines apart. The doctor can help you find better ways to recognize your medicines. Also tell your doctor if you have problems remembering when to take your medicines or how much to take. Your doctor may have some ideas to help, such as a calendar or pill box.
– Swallowing Tablets: If you have trouble swallowing tablets, ask your doctor, nurse, or pharmacist for ideas. Maybe there is a liquid medicine you could use or maybe you can crush your tablets. Do not break, crush, or chew tablets without first asking your health professional.
– Your Lifestyle: If you want to make your medicine schedule more simple, talk about it with your doctor. He or she may have another medicine or ideas that better fits your lifestyle. For example, if taking medicine four times a day is a problem for you, maybe the doctor can give you a medicine you only need to take once or twice a day.
– Put It in Writing: Ask your health care professional to write out a complete medicine schedule, with directions on exactly when and how to take your medicines. Find out from your primary care doctor how your medicine schedule should be changed if you see more than one doctor.
Your Pharmacist Can Help Too
One of the most important services a pharmacist can offer is to talk to you about your medicines. A pharmacist can help you understand how and when to take your medicines, what side effects you might expect, or what interactions may occur. A pharmacist can answer your questions privately in the pharmacy or over the telephone.
Here are some other ways your pharmacist can help:
Many pharmacists keep track of medicines on their computer. If you buy your medicines at one store and tell your pharmacist all the over-the-counter and prescription medicines or dietary supplements you take, your pharmacist can help make sure your medicines don’t interact harmfully with one another.
Ask your pharmacist to place your prescription medicines in easy-to-open containers if you have a hard time taking off child-proof caps and do not have young children living in or visiting your home. (Remember to keep all medicines out of the sight and reach of children.)
Your pharmacist may be able to print labels on prescription medicine containers in larger type, if reading the medicine label is hard for you.
Your pharmacist may be able to give you written information to help you learn more about your medicines. This information may be available in large type or in a language other than English. Your pharmacist can help keep track of your medicines.
To ensure the best possible results from your prescription medications, the following websites
and articles provide more information and suggestions on how to safely use,
store and dispose your Rx meds
Your Medicine: Be Smart. Be Safe.
You can learn more about how to take medicines safely by reading the guide. It answers
common questions about getting and taking medicines and has handy forms that will help
you keep track of information. Keep this guide with your medicines in case you have any
question, concerns, or worries. Use the Wallet Card at the end. This booklet was developed
by NCPIE and the Agency for Healthcare Research and Quality (AHRQ).
View and print Your Medicine: Be Smart. Be Safe. Booklet
Conversation is the Best Medicine
Medicines made easy. Things you need to know about managing your medications
but were afraid to ask. This booklet was developed by the AARP.
View and print Conversation is the best Medicine
Prescription Drug Disposal Locations
Proper disposal of unused or unwanted medications protects the environment,
prevents abuse and reduces accidental poisoning. Here’s a list of permanent
disposal locations where you can safely dispose your unused prescription medications.
Prescription Drug Disposal Locations
Whether you’re a principal, school nurse, teacher, coach, PTSA president or other member of the school community, you can help end the medicine abuse epidemic. Start by educating the teens and parents in your school about the dangers of prescription medicine and over-the-counter cough medicine abuse. Use the free resources below – brochures, posters, a curriculum and more – to raise awareness and to help keep your community healthy and safe.
NIDA for Teens: Parents and Teachers Information and lesson plans from the National Institute on Drug Abuse (NIDA) help teachers engage students about the consequences of drug abuse and addiction. You’ll find “Mind Over Matter”, a teacher’s guide for grades 5-9 to learn about the biological effects of drug abuse, a prescription medicine abuse fact sheet and quiz – along with other drug-related classroom activities.
Not Worth The Risk, Even If It’s Legal: What Educators Need to Know This resource encourages health teachers, coaches, guidance counselors and mentors to have honest conversations with their students and empowers them to play an active role in helping curb teen medicine abuse.